I have put this site together and will continue to add information regarding methemoglobinemia as I acquire it because a relative of mine has a kid who has methemoglobinemia. Frankly, I have never heard of it until they told me about it, and my personal research has opened up an entire world I did not know existed.
Hopefully, what you find here on the site will be of use to you and perhaps save you some time while you look for information for your self regarding this horrible condition. I do not know if this is entirely true or not as it is being told to me second hand and I am not a medical expert, however, my relatives child seems to have gotten methemoglobinemia from drinking contaminated well water.
I have never really thought about people drinking well water and did not even know that people in America did. To my complete surprise many people in all states drink well water. I even met with a guy who specifically works on well water testing and well water repair. He, of course has heard of methemoglobinemia and has stories to tell me. I slowly began to understand how important the work he did.
It is not clear to me yet all the ways you can get methemoglobinemia but one way for a child is to drink contaminated well water. A well contaminated with Nitrated can cause a child to get sick with this condition. There are other ways for people to get sick. Adults can get methemoglobinemia also.
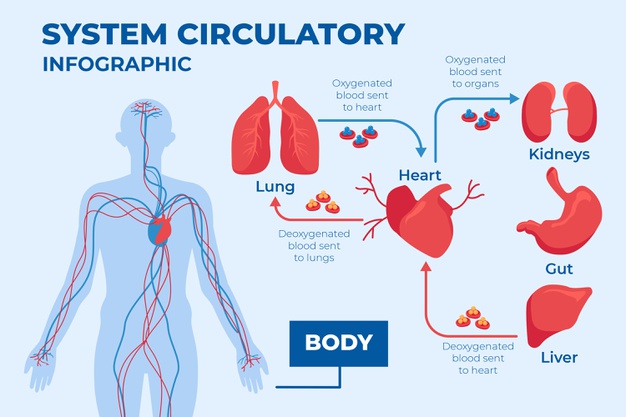
There are treatments for methemoglobinemia, apparently Methylene blue is one way. Because methemoglobinemia effects the bloods ability to carry oxygen, most people also receive oxygen also.
Below is a link to a video on another website which I found very helpful in initially understanding this condition. You will need to give them an email address to sign in and see the video but I feel this video was well worth the time to register. It took a few seconds only and the video speaks English vs Medical and that really helped me understand things quickly. It gets a little technical but is worth the time to watch.
There are two types of inherited MetHb:
• Type 1 (also called erythrocyte reductase deficiency) occurs when RBCs lack the enzyme.
Type 2 (also called generalized reductase deficiency) occurs when the enzyme doesn't work in the body.
The second form of inherited MetHb is called hemoglobin M disease. It is caused by defects in the hemoglobin protein itself. Only one parent needs to pass on the abnormal gene for the child to inherit the disease.
Acquired MetHb is more common than the inherited forms. It occurs in some people after they are exposed to certain chemicals and medicines, including:
• Anesthetics such as benzocaine
• Nitrobenzene
• Certain antibiotics (including dapsone and chloroquine)
• Nitrites (used as additives to prevent meat from spoiling)
Symptoms associated with higher levels of methemoglobin are as follows: 3-15% - Slight discoloration (eg, pale, gray, blue) of the skin. 15-20% - Cyanosis, though patients may be relatively asymptomatic. 25-50% - Headache, dyspnea, lightheadedness (even syncope), weakness, confusion, palpitations, chest pain.
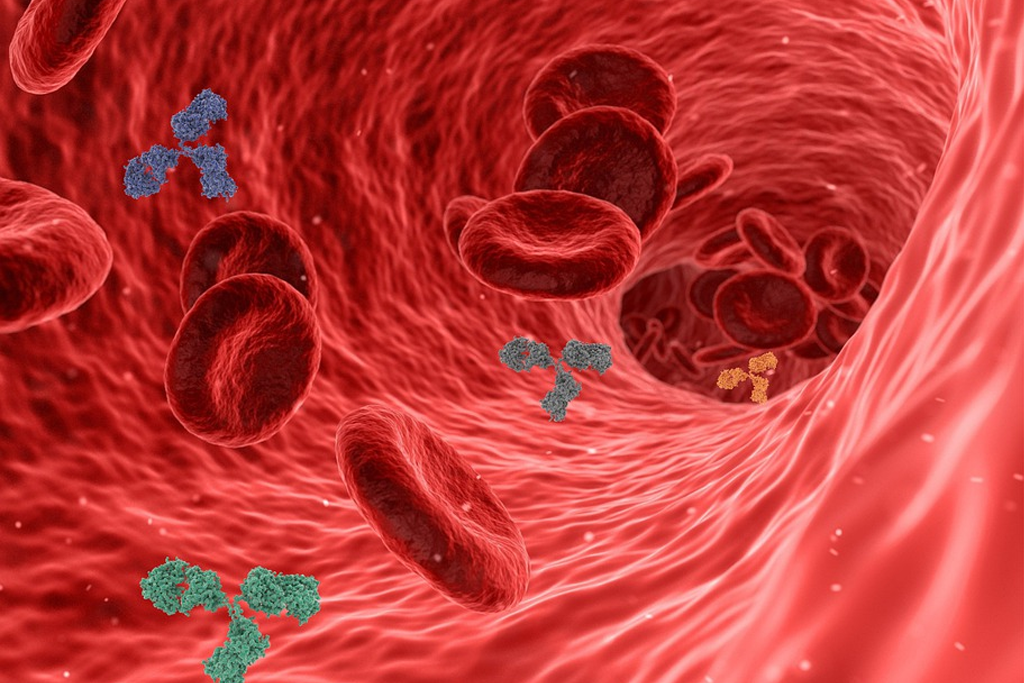
The most common cause of methemoglobinemia, as in this clinical case, is ingestion of or exposure of skin or mucous membranes to oxidizing agents (see box). Some of these oxidize hemoglobin directly to form methemoglobin; others do it indirectly by reducing free oxygen to the free radical O2-, which in turn oxidizes hemoglobin to methemoglobin. Outbreaks of methemoglobinemia have occurred due to nitrite poisoning from water contamination.
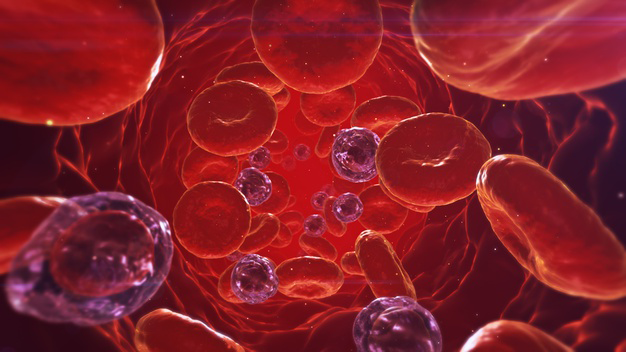
Methemoglobin is a type of hemoglobin. Methemoglobinemia is a blood condition where the patient has abnormal quantities of methemoglobin. Hemoglobin is the molecule that is present in the red blood cells and helps in distributing the oxygen all over the body; whereas, methemoglobin does not have the ability to release oxygen.
Large amounts of nitric oxide are released in patients with sepsis. Nitric oxide is converted to methemoglobin and nitrate. It has been reported that methemoglobin levels are significantly higher in patients with sepsis than in nonseptic patients.
Methemoglobinemia has been reported in young infants (<6 months) in whom severe metabolic acidosis develops from diarrhea and dehydration.7 Young infants may be particularly susceptible to this complication because of their low stomach acid production, large number of nitrite-reducing bacteria, and the relatively easy oxidation of fetal hemoglobin. Small infants have lower erythrocyte levels of cytochrome b reductase.8 Higher intestinal pH of infants may promote the growth of gram-negative organisms that convert dietary nitrates to nitrites.
Symptoms may include headache, dizziness, shortness of breath, nausea, poor muscle coordination, and blue-colored skin (cyanosis). Complications may include seizures and heart arrhythmias.
In otherwise healthy individuals, the protective enzyme systems normally present in red blood cells rapidly reduce the methemoglobin back to hemoglobin and hence maintain methemoglobin levels at less than one percent of the total hemoglobin concentration. Exposure to exogenous oxidizing drugs and their metabolites (such as benzocaine, dapsone, and nitrates) may lead to an increase of up to a thousandfold of the methemoglobin formation rate, overwhelming the protective enzyme systems and acutely increasing methemoglobin levels.
Due to a deficiency of the enzyme diaphorase I (cytochrome b5 reductase), methemoglobin levels rise and the blood of met-Hb patients has reduced oxygen-carrying capacity. Instead of being red in color, the arterial blood of met-Hb patients is brown. This results in the skin of Caucasian patients gaining a bluish hue. Hereditary met-Hb is caused by a recessive gene. If only one parent has this gene, offspring will have normal-hued skin, but if both parents carry the gene, there is a chance the offspring will have blue-hued skin.
Another cause of congenital methemoglobinemia is seen in patients with abnormal hemoglobin variants such as hemoglobin M (HbM), or hemoglobin H (HbH), which are not amenable to reduction despite intact enzyme systems.
 methemoglobinemia A blood disorder in which an abnormal amount of methemoglobin is produced
methemoglobinemia A blood disorder in which an abnormal amount of methemoglobin is produced