I need to do more research on this family called "The Blue People of Kentucky" as I have never heard of them until recently, which of course makes me wonder about what else I have never heard.
The Fugates were a family that lived in the Kentucky hills. This family is also known as the "Blue Fugates" or the "Blue People of Kentucky. It is likely they carried carried a genetic trait that led to the blood disorder methemoglobinemia, which causes the appearance of blue-tinged skin. I cant also help but wonder at the quality of their well water.
The information below comes from a book titled "Human Genetics" by Ricki Lewis.
“A rare but very noticeable condition of abnormal hemoglobin affects the “blue people of Troublesome Creek”. Seven generations ago, in 1820, a French orphan named Martin Fugate who settled in this area of Kentucky brought in an autosomal recessive gene that causes methemoglobinemia. Martin’s mutation was in the CYP5R3 gene, which encodes an enzyme (cytochrome b5 methemoglobin reductase) that normally catalyzes a reaction that converts a type of hemoglobin with poor oxygen affinity, methemoglobin, back into normal hemoglobin by adding an electron. Martin was a heterozygote but still slightly bluish. His wife, Elizabeth Smith, was also a carrier for this very rare disease, and four of their seven children were blue. After extensive inbreeding in the isolated community—their son married his aunt, for example—a large pedigree of “blue people” of both sexes arose.
In “blue person disease,” excess oxygen-poor hemoglobin causes a dark blue complexion. Carriers may have bluish lips and fingernails at birth, which usually lighten. Treatment is simple: A tablet of methylene blue, a commonly used dye adds the electron back to methemoglobin, converting it to normal hemoglobin. In most members of the Fugate family, blueness was the only symptom. Normally, less than 1 percent of hemoglobin molecules are the methemoglobin form, which binds less oxygen. The Fugates had 10 to 20 percent in this form. People with the inherited condition who have more than 20 percent methemoglobin may suffer seizures, heart failure, and even death.”
I cant take credit for this but the following is a youtube video that I feel presents The Blue People story fairly well.
There are two types of inherited MetHb:
• Type 1 (also called erythrocyte reductase deficiency) occurs when RBCs lack the enzyme.
Type 2 (also called generalized reductase deficiency) occurs when the enzyme doesn't work in the body.
The second form of inherited MetHb is called hemoglobin M disease. It is caused by defects in the hemoglobin protein itself. Only one parent needs to pass on the abnormal gene for the child to inherit the disease.
Acquired MetHb is more common than the inherited forms. It occurs in some people after they are exposed to certain chemicals and medicines, including:
• Anesthetics such as benzocaine
• Nitrobenzene
• Certain antibiotics (including dapsone and chloroquine)
• Nitrites (used as additives to prevent meat from spoiling)
Symptoms associated with higher levels of methemoglobin are as follows: 3-15% - Slight discoloration (eg, pale, gray, blue) of the skin. 15-20% - Cyanosis, though patients may be relatively asymptomatic. 25-50% - Headache, dyspnea, lightheadedness (even syncope), weakness, confusion, palpitations, chest pain.
The most common cause of methemoglobinemia, as in this clinical case, is ingestion of or exposure of skin or mucous membranes to oxidizing agents (see box). Some of these oxidize hemoglobin directly to form methemoglobin; others do it indirectly by reducing free oxygen to the free radical O2-, which in turn oxidizes hemoglobin to methemoglobin. Outbreaks of methemoglobinemia have occurred due to nitrite poisoning from water contamination.
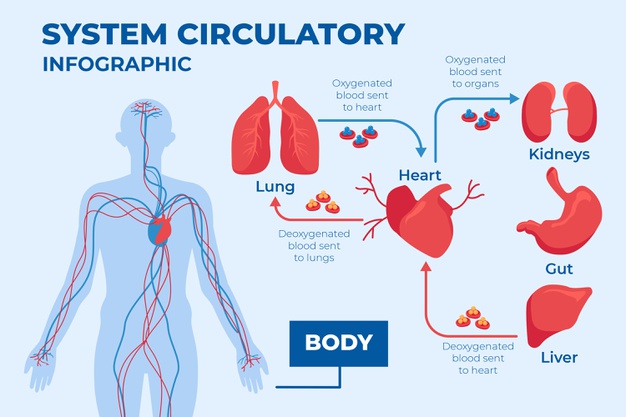
Methemoglobin is a type of hemoglobin. Methemoglobinemia is a blood condition where the patient has abnormal quantities of methemoglobin. Hemoglobin is the molecule that is present in the red blood cells and helps in distributing the oxygen all over the body; whereas, methemoglobin does not have the ability to release oxygen.
Large amounts of nitric oxide are released in patients with sepsis. Nitric oxide is converted to methemoglobin and nitrate. It has been reported that methemoglobin levels are significantly higher in patients with sepsis than in nonseptic patients.
Methemoglobinemia has been reported in young infants (<6 months) in whom severe metabolic acidosis develops from diarrhea and dehydration.7 Young infants may be particularly susceptible to this complication because of their low stomach acid production, large number of nitrite-reducing bacteria, and the relatively easy oxidation of fetal hemoglobin. Small infants have lower erythrocyte levels of cytochrome b reductase.8 Higher intestinal pH of infants may promote the growth of gram-negative organisms that convert dietary nitrates to nitrites.
Symptoms may include headache, dizziness, shortness of breath, nausea, poor muscle coordination, and blue-colored skin (cyanosis). Complications may include seizures and heart arrhythmias.
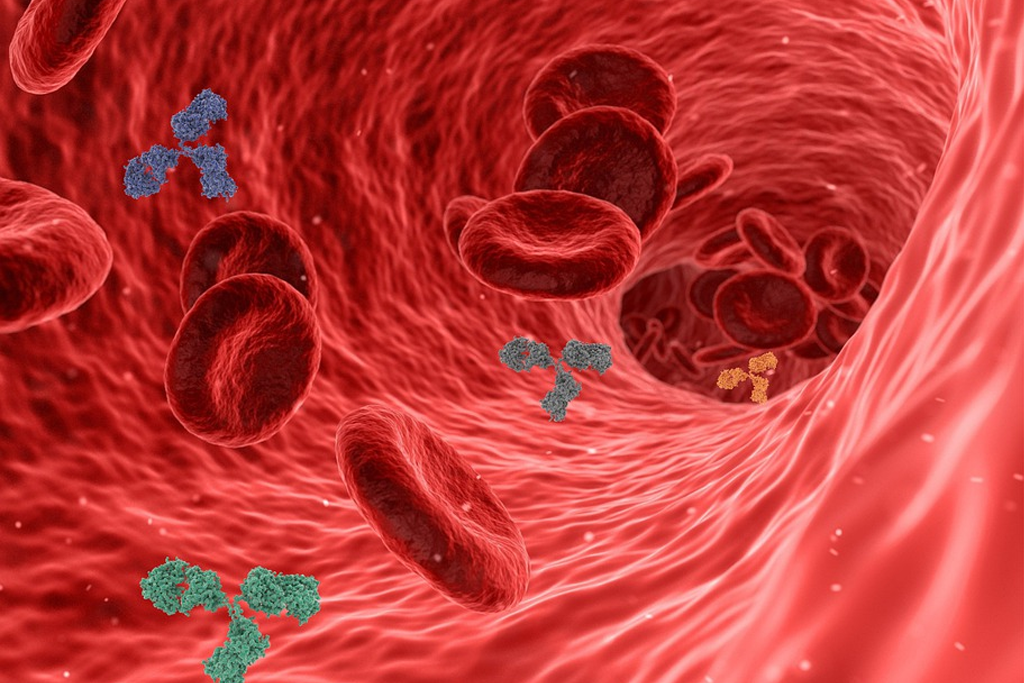
In otherwise healthy individuals, the protective enzyme systems normally present in red blood cells rapidly reduce the methemoglobin back to hemoglobin and hence maintain methemoglobin levels at less than one percent of the total hemoglobin concentration. Exposure to exogenous oxidizing drugs and their metabolites (such as benzocaine, dapsone, and nitrates) may lead to an increase of up to a thousandfold of the methemoglobin formation rate, overwhelming the protective enzyme systems and acutely increasing methemoglobin levels.
Due to a deficiency of the enzyme diaphorase I (cytochrome b5 reductase), methemoglobin levels rise and the blood of met-Hb patients has reduced oxygen-carrying capacity. Instead of being red in color, the arterial blood of met-Hb patients is brown. This results in the skin of Caucasian patients gaining a bluish hue. Hereditary met-Hb is caused by a recessive gene. If only one parent has this gene, offspring will have normal-hued skin, but if both parents carry the gene, there is a chance the offspring will have blue-hued skin.
Another cause of congenital methemoglobinemia is seen in patients with abnormal hemoglobin variants such as hemoglobin M (HbM), or hemoglobin H (HbH), which are not amenable to reduction despite intact enzyme systems.
 methemoglobinemia A blood disorder in which an abnormal amount of methemoglobin is produced
methemoglobinemia A blood disorder in which an abnormal amount of methemoglobin is produced
